
Weighing the
Disease Burden
Actual patient living with HS
Hidradenitis suppurativa. HS. It’s an agonizing, devastating disease that can severely impact not just quality of life but many aspects of life for those who live with it. Early detection, intervention, and capturing the window of opportunity is therefore critical to helping to prevent irreversible damage from this devastating disease.
1 out of every 100,000 people in the US has been diagnosed with HS.1 But the precise prevalence of HS is difficult to understand because of extensive delays in diagnosis—delays that can carve away 10 years from a patient’s life on average.2-4
Average time from symptom onset to HS diagnosis2:
10 years
YEAR 1
Begins university
programYEAR 2
Painful blemishes start forming
YEAR 3
Visits university health center
Dx = FolliculitisCondition worsening—feels something more serious is going onYEAR 4
Experiences first major flareYEAR 5
Visits ER and receives pain medications, antibiotics, and referral to dermatologist
Dx = CarbunculosisPain becoming crippling—missing classes- YEAR 6
YEAR 7
Feelings of isolation increase and mental health declinesGraduates but skips celebrations- YEAR 8
YEAR 9
Frustrated by minimal disease improvement Visits dermatologist
Visits dermatologist
Dx = Adult onset body acne
Dx = diagnosis.
Often more than 3 misdiagnoses along the way.3
HS manifestation can include3:
- Recurring inflammatory nodules
- Abscesses
- Draining fistulas
- Scars
To make matters worse, symptoms can3,5-7:
- Be unpredictable
- Be variable
- Lead to permanent disfigurement from scarring and tunneling
Beyond the visual, visceral impact of scarring, HS can make physical function almost impossible when scars create limb contractures that lead to limited movement.3
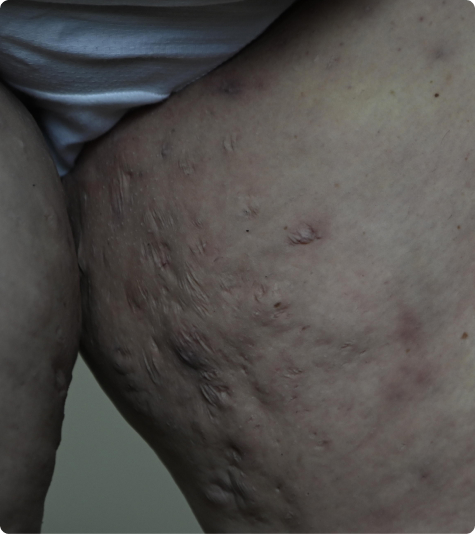
Actual patient living with HS
HS has the power to permanently change a person’s body and life.
Recurrent flares can derail work and lead to social, emotional, and psychological devastation.5,8,9 Adding to the dilemma, diminished self-esteem and increased isolation make HS patients more prone to self-destructive behaviors.10
HS Scars: Seen and Unseen
Social withdrawal or isolation11
Among those living with HS ...

41.3%
quit spending time with family

60%
stopped hobbies

66.1%
experienced a diminished social life
Diminished intimacy
Sexual Quality of Life
Questionnaire (SQoL) for Men12

A lower score on the SQoL indicates a lower sexual quality of life.
Female Sexual Distress
Scale-Revised (FSDS-R)12

A higher score on the FSDS-R indicates higher sexual distress for females.
Financial strain and unemployment9
On average, patients with HS ...
Lose up to 7 workdays a year because of HS13
Take ~4 more days off (medical and disability absenteeism) than those without HS14
Spend $1,317 more in medical absenteeism and disability costs vs those without HS14
Substance use disorder (SUD)
Compared to those without HS, twice as many people with HS misuse substances (4.0% vs 2.0%)15

29.7%
Cannabis15

32.7%
Opioids15

47.9%
Alcohol15
HS often presents with multiple physical and psychosocial comorbidities that can add to the burden of disease management.16
- Acne vulgaris
- Dissecting cellulitis of the scalp
- Pilonidal cyst
- Pyoderma gangrenosum
- Depression and anxiety
- Tobacco use
- Polycystic ovary syndrome (PCOS)
- Inflammatory bowel disease
A comprehensive management plan should include ways to address comorbidities that impact disease development or progression.17
References
- Jfri A, Nassim D, O’Brien E, et al. Prevalence of hidradenitis suppurativa: a systematic review and meta-regression analysis. JAMA Dermatol. 2021;157(8):924-931.
- Garg A, Neuren E, Cha D, et al. Evaluating patients’ unmet needs in hidradenitis suppurativa: results from the Global Survey Of Impact and Healthcare Needs (VOICE) Project. J Am Acad Dermatol. 2020;82(2):366-376.
- Kokolakis G, Wolk K, Schneider-Burrus S, et al. Delayed diagnosis of hidradenitis suppurativa and its effect on patients and healthcare system. Dermatology. 2020;236(5):421-430.
- Hendricks AJ, Hsiao JL, Lowes MA, Shi VY. A comparison of international management guidelines for hidradenitis suppurativa. Dermatology. 2021;237(1):81-96.
- Sabat R, Jemec GBE, Matusiak Ł, et al. Hidradenitis suppurativa. Nature Reviews Disease Primers. 2020;6(1):18.
- Schneider-Burrus S, Tsaousi A, Barbus S, et al. Features associated with quality of life impairment in hidradenitis suppurativa patients. Front Med (Lausanne). 2021;8:676241.
- Lee EY, Alhusayen R, Lansang P, et al. What is hidradenitis suppurativa? Can Fam Physician. 2017;63(2):114-120.
- Huang CM, Kirchhof MG. Hidradenitis suppurativa from a patient perspective including symptoms and self-treatment. J Cutan Med Surg. 2021;25(6):591-597.
- Matusiak Ł. Profound consequences of hidradenitis suppurativa: a review. Br J Dermatol. 2020;183(6):e171-e177.
- Głowaczewska A, Reszke R, Szepietowski JC, Matusiak Ł. Indirect self-destructiveness in hidradenitis suppurativa patients. J Clin Med. 2021;10(18).
- Perche PO, Singh R, Senthilnathan A, Feldman SR, Pichardo RO, et al. Hidradenitis suppurativa’s impact on social activities: an observational study. Cureus. 2022;14(5):e25292.
- Alavi A, Farzanfar D, Rogalska T, et al. Quality of life and sexual health in patients with hidradenitis suppurativa. Int J Women’s Dermatol. 2018;4(2):74-79.
- Jemec GB, Heidenheim M, Nielsen NH. Hidradenitis suppurativa—characteristics and consequences. Clin Exp Dermatol. 1996;21(6):419-423.
- Tzellos T, Yang H, Mu F, et al. Impact of hidradenitis suppurativa on work loss, indirect costs and income. Br J Dermatol. 2018;181(1):147-154.
- Garg A, Papagermanos V, Midura M, et al. Opioid, alcohol, and cannabis misuse among patients with hidradenitis suppurativa: a population-based analysis in the United States. J Am Acad Dermatol. 2018;79(3):495-500.e491.
- Garg A, Malviya N, Strunk A, et al. Comorbidity screening in hidradenitis suppurativa: evidence-based recommendations from the US and Canadian Hidradenitis Suppurativa Foundations. J Am Acad Dermatol. 2022;86(5):1092-1101.
- Alikhan A, Sayed C, Alavi A, et al. North American clinical management guidelines for hidradenitis suppurativa: a publication from the United States and Canadian Hidradenitis Suppurativa Foundations: part II: topical, intralesional, and systemic medical management. J Am Acad Dermatol. 2019;81(1):91-101.

