Personalizing Treatment Begins With Recognizing the Window of Opportunity
Actual patient living with HS

Actual patient living with HS
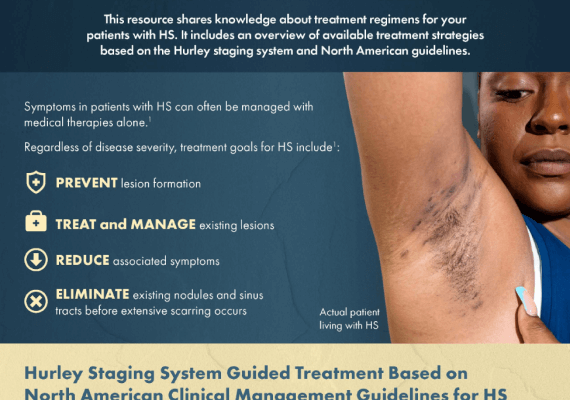
HS guidelines empower healthcare providers to determine appropriate strategies for achieving patient treatment goals and improving quality of life.1-3
As HS is a progressive disease, therapeutic regimens should be individualized for each patient with consideration of 4,5:
- Disease severity
- Psychosocial impact
- Symptomology
Because of its impact on everyday life, the severity of pain must be considered when determining the right management modalities for HS.6,7
Patients with HS will benefit most from a multidisciplinary care team of dermatologists, primary care healthcare providers, gynecologists, psychiatrists, pain management teams, and surgeons.3
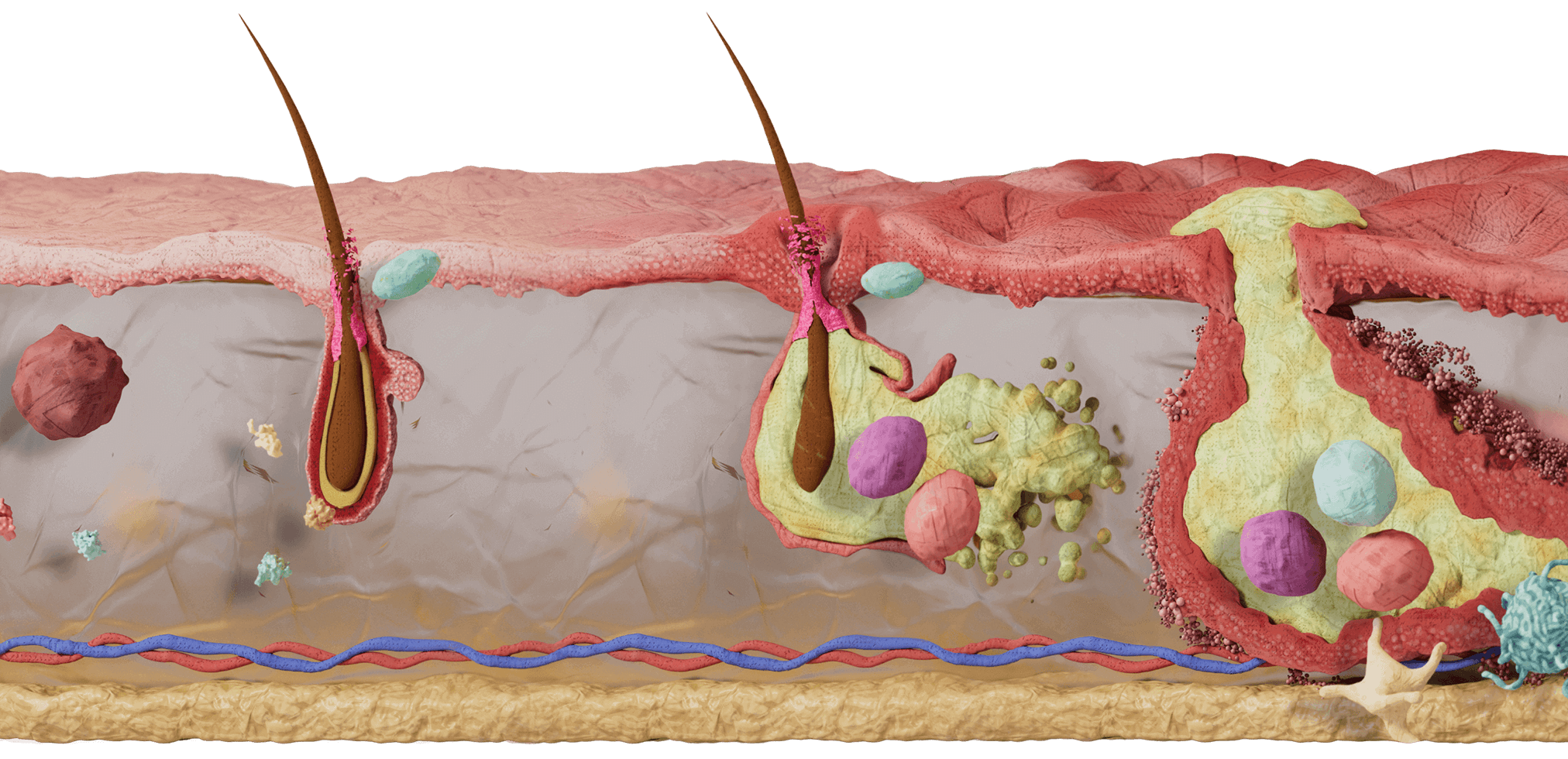
Window of opportunity:
Alter the natural HStory of the disease
Addressing HS early, when anti-inflammatory attempts will be most effective, can decrease progression and may alter the natural HStory of the disease.8 The optimal time for treating HS and improving clinical outcomes is before irreversible damage and development of lesions such as fistulas, sinus tracts, and scarring has occurred.8,9 This is called the “window of opportunity.”
Window of Opportunity
Disease Progression
Early Disease
Moderate Disease
Late Disease
In addition to HS, the concept of the window of opportunity has been studied in other immune-mediated disease states such as rheumatoid arthritis (RA) and Crohn’s disease (CD).10-12
In fact, the term “window of opportunity” has been used in RA for over 30 years.10 It is considered a period early in a disease when the underlying mechanism is not fully developed, so therapeutic modification of the disease may be more successful.11
Looking at early RA outcome data and symptom duration* at treatment initiation, a systematic review of randomized controlled trials and cohort studies found significant evidence to support a window of opportunity, showing that those with longer symptom duration had a decreased chance of disease-modifying antirheumatic drug (DMARD)-free remission.11
Similarly, evidence suggests treating CD during the window of opportunity with disease-modifying agents, such as biologics, can aid in achieving disease remission and preventing bowel damage.12 Early initiation of biologics is therefore recommended in CD to prevent long-term disease outcomes and improve patient quality of life.12
This window of opportunity allows patients to receive treatment with immunomodulatory therapies as early in the disease state as possible—before irreversible damage has occurred.
*Symptom duration was defined as the period between symptom onset and start of treatment.
Treatment Options1,3-5
HS treatment can be personalized based on disease severity, socioeconomic factors, and patient preference.
Use of this resource is not intended to be a substitute for, or an influence on, your independent medical judgment. Please exercise your medical discretion when diagnosing and treating your patient’s medical condition. UCB does not offer personalized medical diagnosis or patient-specific advice.
Topical and intralesional therapies
- Skin cleansers
- Keratolytic agents
- Topical antibiotics (topical clindamycin)1,13
Systemic antibiotics
The role of antibiotics in HS4 is uncertain, as they don’t achieve prolonged disease remission or prevention of disease progression. They also come with high recurrence of disease activity post discontinuation.4,13
Monotherapy is primarily used for mild disease because of its lower response and increased disease recurrence in more advanced stages.1
Systemic antibiotics may be used as adjunctive therapy in moderate-to-severe HS1–but only with careful consideration of risk versus benefit.
Biologic therapies
Tumor necrosis factor (TNF) and interleukins (e.g., IL-1, IL-12, IL-17A, and IL-17F) are examples of biologic therapy targets for HS treatment.1,14
Other pharmacological therapies
- Oral retinoids
- Hormonal therapies
- Systemic immunosuppressants (e.g., steroids)
- Pain management
Making healthy choices every day can help patients manage their HS and its associated comorbidities.3,4
- Smoking cessation
- Weight loss
- Shaving adaptations
- Antiperspirants
- Wound care
- Incision and drainage
- Deroofing
- Excision
- Laser therapy
Let’s listen to how Cydney’s HS was managed—and review HS management with dermatologists Dr. Jennifer Hsiao and Dr. Hadar Lev-Tov.
Pain management is an unavoidable and unquestionable HS treatment goal
Use of this resource is not intended to be a substitute for, or an influence on, your independent medical judgment. Please exercise your medical discretion when diagnosing and treating your patient’s medical condition. UCB does not offer personalized medical diagnosis or patient-specific advice.
Acute pain-relief strategies15
- Individual lesion incision and drainage
- Topical lidocaine, oral acetaminophen, oral nonsteroidal anti-inflammatory drugs (NSAIDs), and intralesional triamcinolone
- Short-acting opiates may be used with caution
Chronic pain-relief strategies
- The American Academy of Dermatology-recommended World Health Organization Pain Ladder starts with the least-invasive medical therapy and increases therapeutic intensity as needed.16,17
- Neuromodulatory medications, including pregabalin, gabapentin, serotonin-norepinephrine reuptake inhibitors (SNRIs) and tricyclic antidepressants (TCAs), may improve neuropathic pain.15
- For severe refractory pain that requires higher-risk pharmacotherapy and procedures, a pain management specialist should be consulted.15
- Collaborating with behavioral health experts and using psychological treatments that teach coping skills, such as cognitive behavioral therapy (CBT) and acceptance and commitment therapy (ACT), are essential to HS pain care.15
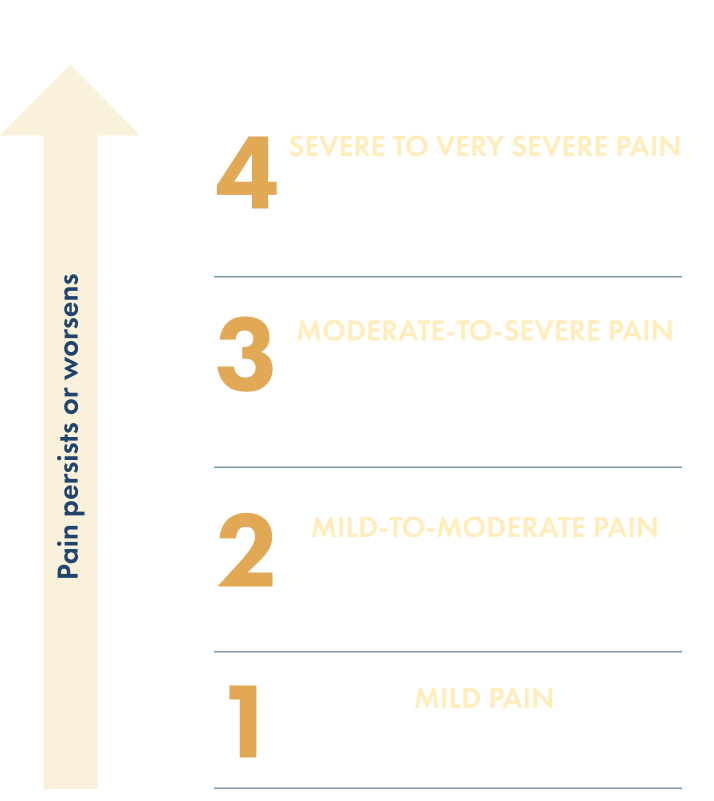
According to the World Health Organization pain ladder, “strong opioids” include morphine, oxycodone, methadone, hydromorphone, and fentanyl; “weak opioids” include codeine, hydrocodone, and tramadol.16 However, the overall profile of the opioid and individual patient factors should be considered, starting with a low dose and titrating as required.16
Patients want something more, something better, and they want it earlier
Appropriate immunomodulating therapy may help prevent patients with moderate-to-severe HS from taking urgent measures to self-treat when antibiotics and topicals don’t give them their desired outcome or help with the underlying inflammation that drives the disease.7,18,19 Patients have reported self-treatment of their lesions through various methods, such as squeezing, soaking, and even lancing.7
Addressing HS during the “window of opportunity,” when anti-inflammatory attempts will be most effective, may alter the natural HStory of the disease.8
A better understanding of the underlying pathophysiology of HS is essential to effectively managing the disease and developing a comprehensive standard of care.20
See HS pathophysiology
Actual patient living with HS
References
- Alikhan A, Sayed C, Alavi A, et al. North American clinical management guidelines for hidradenitis suppurativa: a publication from the United States and Canadian Hidradenitis Suppurativa Foundations: part II: topical, intralesional, and systemic medical management. J Am Acad Dermatol. 2019;81(1):91-101.
- Zouboulis CC, Desai N, Emtestam L, et al. European S1 guideline for the treatment of hidradenitis suppurativa/acne inversa. J Eur Acad Dermatol Venereol. 2015;29(4):619-644.
- Hendricks AJ, Hsiao JL, Lowes MA, Shi VY. A comparison of international management guidelines for hidradenitis suppurativa. Dermatology. 2021;237(1):81-96.
- Sayed CJ, Hsiao JL, Okun MM, Hidradenitis Suppurativa Foundation Women's Health Subcommittee. Clinical epidemiology and management of hidradenitis suppurativa. Obstet Gynecol. 2021;137(4):731-746.
- Lee EY, Alhusayen R, Lansang P, et al. What is hidradenitis suppurativa? Can Fam Physician. 2017;63(2):114-120.
- Kokolakis G, Wolk K, Schneider-Burrus S, et al. Delayed diagnosis of hidradenitis suppurativa and its effect on patients and healthcare system. Dermatology. 2020;236(5):421-430.
- Huang CM, Kirchhof MG. Hidradenitis suppurativa from a patient perspective including symptoms and self-treatment. J Cutan Med Surg. 2021;25(6):591-597.
- Martorell A, Jfri A, Ochando G, et al. Present and future trends of biologic therapies and small molecules in hidradenitis suppurativa. J IMIDs. 2022;2(1):8-19.
- Marzano AV, Genovese G, Casazza G, et al. Evidence for a “window of opportunity” in hidradenitis suppurativa treated with adalimumab: a retrospective, real-life multicentre cohort study. Br J Dermatol. 2021;184(1):133-140.
- Burgers LE, Raza K, van der Helm-van Mil AH. Window of opportunity in rheumatoid arthritis - definitions and supporting evidence: from old to new perspectives. RMD Open. 2019;5(1):e000870.
- van Nies JA, Krabben A, Schoones JW, Huizinga TW, Kloppenburg M, van der Helm-van Mil AH. What is the evidence for the presence of a therapeutic window of opportunity in rheumatoid arthritis? A systematic literature review. Ann Rheum Dis. 2014;73(5):861-870.
- Danese S, Fiorino G, Fernandes C, Peyrin-Biroulet L. Catching the therapeutic window of opportunity in early Crohn's disease. Curr Drug Targets. 2014;15(11):1056-1063.
- van der Zee H, Bunte M, Straalen K. Management of mild hidradenitis suppurativa: our greatest challenge yet. Br J Dermatol. 2022;186(2):355-356.
- Fletcher JM, Moran B, Petrasca A, Smith CM. IL-17 in inflammatory skin diseases psoriasis and hidradenitis suppurativa. Clin Exp Immunol. 2020;201(2):121-134.
- Savage KT, Singh V, Patel ZS, et al. Pain management in hidradenitis suppurativa and a proposed treatment algorithm. J Am Acad Dermatol. 2021 Jul;85(1):187-199.
- Pergolizzi J, Raffa R. The WHO pain ladder: do we need another step? Pract Pain Manag. 2014;14(1).
- Alikhan A, Sayed C, Alavi A, et al. North American clinical management guidelines for hidradenitis suppurativa: a publication from the United States and Canadian Hidradenitis Suppurativa Foundations: part I: diagnosis, evaluation, and the use of complementary and procedural management. J Am Acad Dermatol. 2019;81(1):76-90.
- Garg A, Neuren E, Cha D, et al. Evaluating patients’ unmet needs in hidradenitis suppurativa: results from the Global Survey of Impact and Healthcare Needs (VOICE) Project. J Am Acad Dermatol. 2020;82(2):366-376.
- Garg A, Naik HB, Kirby JS. A practical guide for primary care providers on timely diagnosis and comprehensive care strategies for hidradenitis suppurativa. Am J Med. 2022;136(1):42-53.
- van Straalen KR, Ingram JR, Augustin M, Zouboulis CC. New treatments and new assessment instruments for hidradenitis suppurativa. Exp Dermatol. 2022;31(Suppl 1):33-39.