
Resources to help you make HStory
We offer these resources for you to share with your patients as you discuss HS in detail. You’ll find material covering everything from diagnosis and comorbidities to facts and fiction, along with FAQs. Use these pieces to highlight specific points—and emphasize that HS is manageable.
Resources for you

DETERMINING the DIAGNOSIS:
HS Questionnaire + Screening Tool
A helpful resource to assess and evaluate a patient for HS.
DOWNLOAD PDF (en)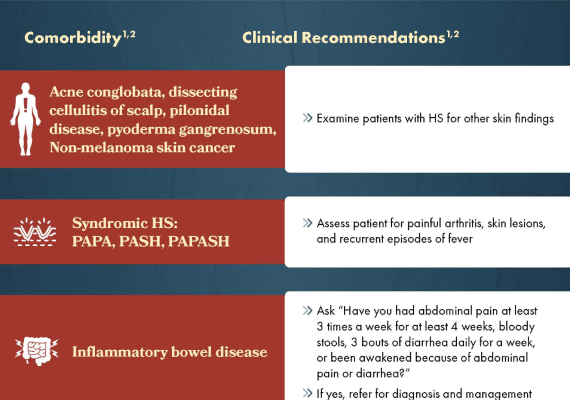
HS DOESN’T GO SOLO:
Comorbidities Associated With HS
A list of comorbidities that can accompany HS.
DOWNLOAD PDF (en)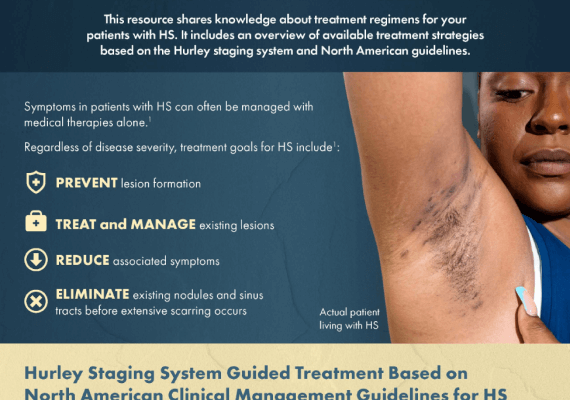
MILD-MODERATE-SEVERE:
Managing HS Stages
A resource that highlights treatment options for HS.
DOWNLOAD PDF (en)Resources for you and your patient
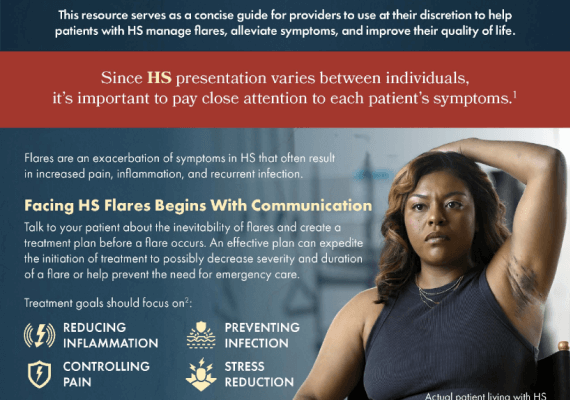
FLARE CARE:
HS Toolkit
Material about recognizing and treating flares along with templates for at-home care plans.
DOWNLOAD PDF (en) DOWNLOAD PDF (es)
FACT vs. FICTION:
HS Truths
What’s accurate about HS? What’s not? A checklist to review with patients.
DOWNLOAD PDF (en) DOWNLOAD PDF (es)
NOT JUST PAINFUL BUMPS:
HS FAQs
A list of the most common questions and answers about HS.
DOWNLOAD PDF (en) DOWNLOAD PDF (es) HS in Words & Pictures
Misunderstanding Hidradenitis Suppurativa (HS)
Focus on Flare-ups
Managing Hidradenitis Suppurativa (HS): Modalities and Medicines
Living With HS: Cydney's Story
Sharing Her Story
Discovering the Diagnosis
Managing HS
Managing HS Pain
Resources for Managing the Impact of HS
Occlusion and Dilation of Hair Follicle: Hidradenitis suppurativa lesions primarily occur after the occlusion of a hair follicle (follicular hyperkeratosis) triggers a dysregulated innate and adaptive inflammatory response of apocrine glands causing dilation of the hair follicles. Initially a mild disease state.1,2
IL=interleukin. Th=T helper. TNF=tumor necrosis factor.
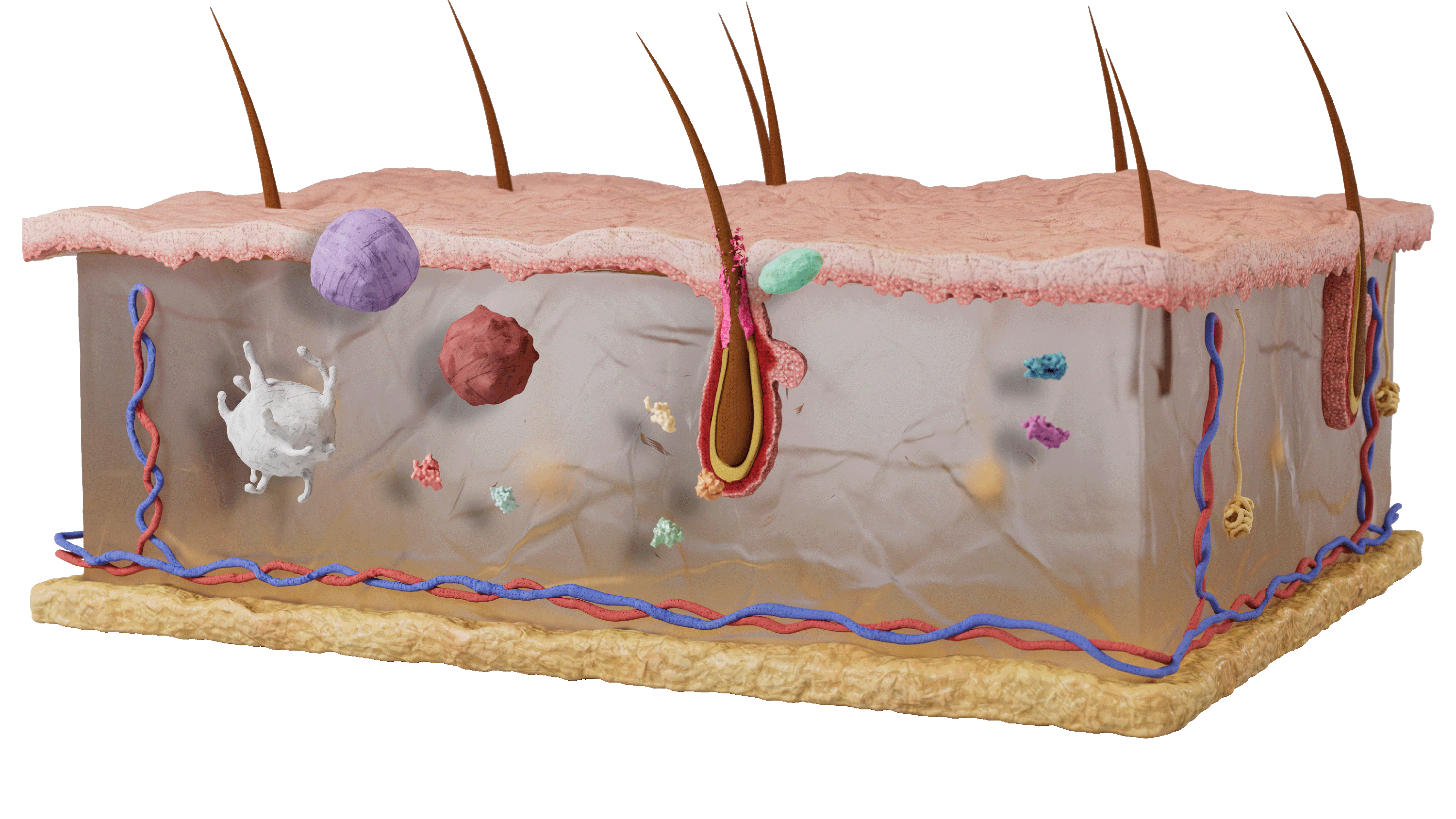
In non-lesional HS, increased Th17 non-inflammatory immune surveillance is present.3
Exogenous factors cause dysbiosis of the microbiome around the hair follicle, which stimulates keratinocytes to start an inflammatory cascade. Genetic factors cause dysregulation of this adaptive immune response, resulting in an autoimmune response and uncontrolled release of pro-inflammatory cytokines.3
Follicular hyperkeratosis causes follicular occlusion, dilation, and rupture.4
IL-23 stimulates CD4+ T-cells to become Th17 cells which produce IL-17A and F. These cytokines induce the IL-1B, IL-6, and TNF-α leading to more hyperkeratosis, inflammation, and follicular obstruction.1,2
Follicular Rupture and Abscess Formation: IL-17 A/F, amongst other inflammatory cytokines, induce the expression of a broad range of proinflammatory chemokines including CXCL1/6/8 and GCSF. This drives neutrophil migration to the follicular site. Granulocyte, T-cell, B-lymphocyte, plasma cell, and monocyte (macrophage and dendritic cell) infiltration leads to follicular rupture and inflammatory nodule and abscess formation at which point the disease is considered moderate.1,2
CXCL=chemokine (C-X-C motif) ligand. GCSF=granulocyte colony-stimulating factor.
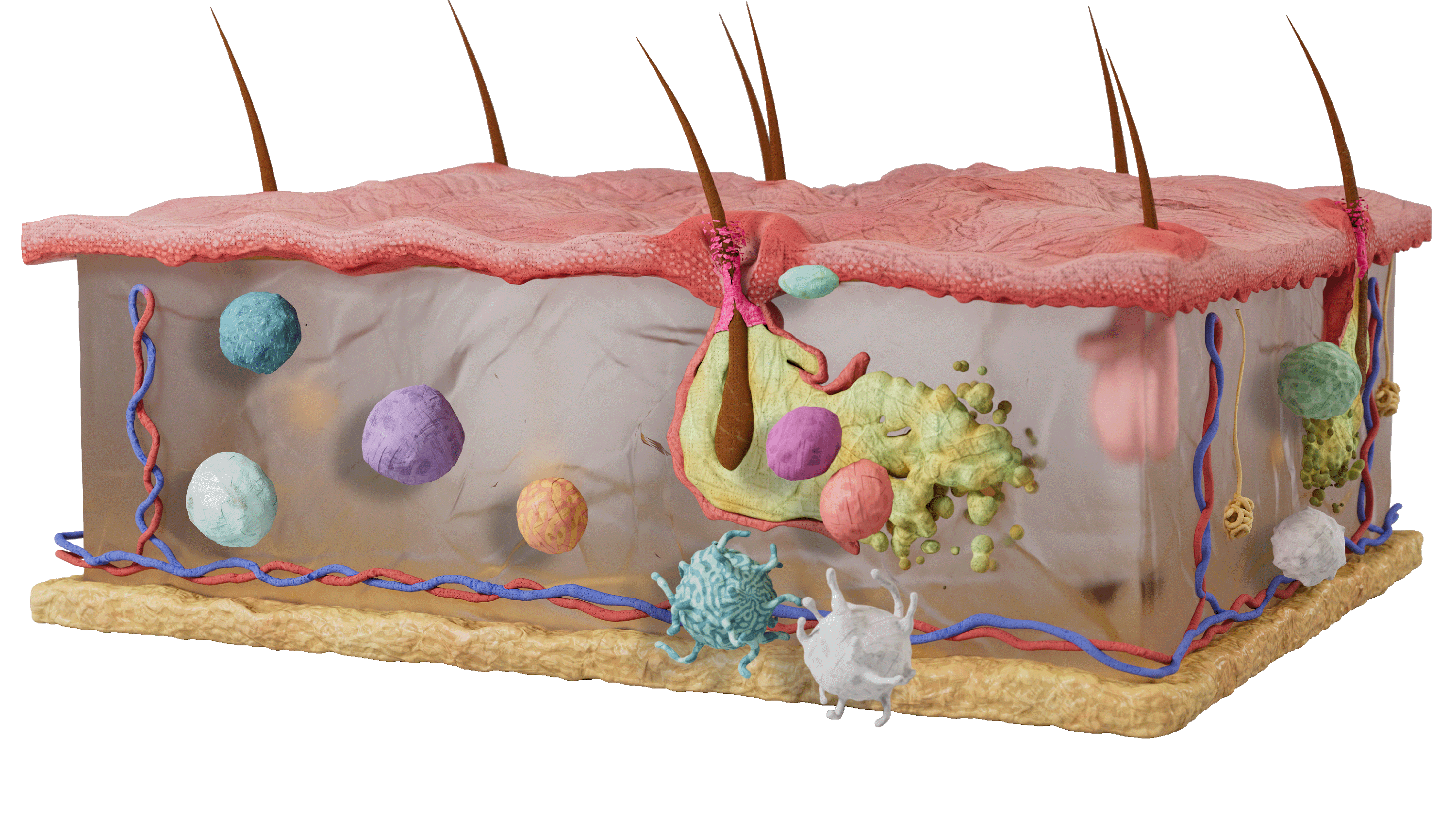
Follicular clogging leads to pilosebaceous and sweat gland changes, cytokine propagation, and inflammation cause follicular rupture and inflammatory nodules and abscess formation.2,4
Perifollicular cellular infiltrate results in abscess formation and destruction of the pilosebaceous unit.1
Chronic Inflammation: Severe HS occurs when chronic inflammation and the imbalance of fibrotic factors cause scarring and sinus tract formation.1

Th17 cells found in HS tissue are associated with epidermal psoriasiform hyperplasia and transepithelial neutrophil migration along tunnel epithelium.3
Fibroblasts contribute to the development of tunnels and epithelialized tracts and fibrosis of HS scars.5
Epithelialized dermal tunnels become pathways for newly recruited inflammatory cell.3
References
- Scala E, Cacciapuoti S, Garzorz-Stark N, et al. Hidradenitis suppurativa: where we are and where we are going. Cells. 2021;10(8):1-19.
- Wolk K, Join-Lambert O, Sabat R. Aetiology and pathogenesis of hidradenitis suppurativa. Br J Dermatol. 2020;183(6):999-1010.
- Zouboulis CC, Benhadou F, Byrd AS, et al. What causes hidradenitis suppurativa? 15 years after. Exp Dermatol. 2020;29(12):1154-1170.
- Goldburg SR, Strober BE, Payette MJ. Hidradenitis suppurativa: epidemiology, clinical presentation, and pathogenesis. J Am Acad Dermatol. 2020;82(5):1045-1058.
- Frew JW, Navrazhina K, Marohn M, et al. Contribution of fibroblasts to tunnel formation and inflammation in hidradenitis suppurativa/acne inversa. Exp Dermatol. 2019;28(8):886-891.